Figure 1. PRISMA article selection flowchart.
Volume 20, Number 2
Abdullahi Abubakar Yunusa1,2, Irfan Naufal Umar2, and Brandford Bervell2,3
1Usmanu Danfodiyo University Sokoto, Nigeria, 2Centre for Instructional Technology and Multimedia, Universiti Sains Malaysia, Malaysia, 3College of Distance Education, University of Cape Coast, Ghana
Medical education in Africa is in desperate need of reforms, evident in widespread diseases, and an inability to mobilise and train the required medical workforce to deal with these health issues. However, the exponential rise in the use of mobile technologies due to the spread of the Internet and increased telecommunication networks offer an opportunity for the transformation of medical education and practice through the deployment of mobile devices as a medium for learning and conveying health care services to the remote and resource-constrained locations of Sub-Saharan Africa (SSA). This paper reviewed articles on the affordances of m-learning for distributed medical education in SSA published between 2010-2018. Results from 18 articles identified in the review revealed a slow-paced ascendancy of practice and research in the field; it further exposed competing priorities, infrastructural deficit, and chronic workforce shortages as the bane of m-learning implementation in the subregion. This paper makes recommendations that will enhance the growth of mobile-based distance medical education and practice in SSA.
Keywords: mobile learning, distributed learning, medical education, Sub-Saharan Africa
Globally, the advent of the Internet has led to a progressive transformation in all facets of human activities. Amongst these, is the impact of Internet-driven technologies that have reshaped the educational landscape. It has become apparent that the traditional form of teaching and learning confined to the classroom is no longer efficient due to limited out of class collaboration and inadequate infrastructure (Africa-America Institute (AAI), 2015; Organisation for Economic Co-operation and Development (OECD), 2009). However, electronic learning (e-learning) has the affordances to accommodate more people, especially those with limited access to regular schooling (Yunusa & Dalhatu, 2014) as an alternative medium to education. The increasing rate of the remote and mobile workforce has resulted in the emergence of the use of mobile technologies for communication, collaboration, and exchange of occupational knowledge practices and training. Consequently, this has evolved into various forms of technology-enhanced learning solutions across human endeavour and the ubiquity of mobile devices for mobile learning is now potentially more revolutionary than e-learning (Okai-Ugbaje, Ardzejewska, & Ahmed, 2017).
Keegan (as cited in Ally, 2009) predicted that the future of mobile learning is “wireless,” and today virtually all human activities are gradually transforming into online using several mobile devices and platforms. Sub-Saharan Africa (SSA) has the most significant number of adolescents and young adults in the world. The International Telecommunication Union (ITU) report (2016) on mobile cellular penetration indicate a mobile penetration rate of 65% in SSA. Relatedly, Masita-Mwangi, Mwakaba, Ronoh-Boreh and Impio (2012) note that 43% of the population in SSA is below the age of 15 years making the region the youngest region in the world. Consequent upon which many African countries are making efforts in widening access and creating opportunities for the expansion of the Higher Education institutions to accommodate these young adults. However, these efforts are ineffective due to the rising number of students with an average of 50% more students per professor in African universities compared to the global average AAI (as cited in Bervell & Umar, 2017).
One key aspect of education in sub-Saharan Africa that needs a technological intervention due to the problem above is medical education. The use of mobile learning offers opportunities for training more medical staff and promoting distance-based medical practices in Sub-Saharan Africa. Recently, authors such as Chaya, Pilot, and Urassa (2018); Lazarus, Sookrajh, and Satyapal (2017a) and Witt et al. (2016) had echoed the need for reforms in medical education and practice in SSA when they suggested the mobile learning paradigm. Recognising the need for mobile learning, these African medical practitioners have suggested that the adoption of mobile technologies and online courses will enable class sizes to increase dramatically in a short space of time and could potentially be significant in mobilising a medical workforce that is struggling with traditional modalities that cannot produce the desired results. The growth of these technologies across the world and Africa, in particular, has prompted some studies on the use of mobile devices in medical education in SSA (Adebara, Adebara, Olaide, Emmanuel, & Olanrewaju, 2017; Chaya, Pilot, & Urassa, 2018; Frehywot et al., 2013; Ibrahim, Salisu, Popoola, & Ibrahim 2014; Lazarus, Sookrajh, & Satyapal, 2017b; Masika et al., 2015; Witt et al., 2016b).
Koole (2009) defines mobile learning as “a process resulting from the convergence of mobile technologies, human learning capacities, and social interaction” (p.25). Accordingly, this definition placed m-learning within four central constructs namely, technological tools, context and social interactions buttressed by Krull and Duart (2017) and Naismith, Lonsdale, Vavoula, and Sharples (2004). Tsinakos and Ally (2013) explain m-learning as “the processes of coming to know through conversations across multiple contexts amongst people and personal interactive technologies” (p. 225). Mobile medical education referred to as mobile health education (m-health) is the process in which smartphones are used to help educate and inform students in the medical field (Ayemoba, 2017). According to Urassa et al. (2018), m-health is an emerging trend in the Health Information System, and defined as the use of mobile technology, such as cellular phones, wireless devices, or radio frequency identification tags, for health care or health services.
Despite the growing amount of research on m-learning in Higher Education across the world (Kaliisa & Picard, 2017; Koole, 2009; Krull & Duart 2017; Tsinakos & Ally, 2013) there are few studies on its use in promoting medical education and practice in Sub-Saharan Africa. The World Health Organization (WHO) (2011) conducted a global survey on the explosion of m-health and telemedicine activities around the world. Even though the report provided some extracts on efforts at using mobile technologies to deliver health services and information to remotely located and resource-constrained communities, the outcome of this report indicated that out of the 114 countries surveyed, SSA had the least positive indices on initiatives in m-learning in medical education (WHO, 2011). Against this background, this paper reviewed published articles based on studies carried out in the subregion between 2010-2018, bringing to fore the trends, milestones, and barriers to effective implementation of mobile technology-based learning solutions in medical education and contributes a reference that will guide policy and practice in the subregion.
Forthrightly, the study sought to answer the following questions:
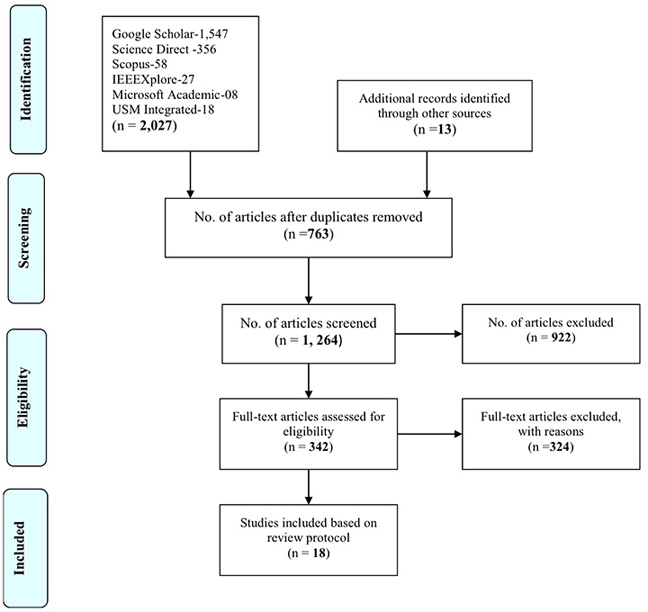
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol by Moher, Liberati, Tetzlaff, Altman, and Prisma Group. (2009). The PRISMA protocol is a step-by-step process to search, collect, analyse, synthesise, and report findings from the literature (see Figure 1). The first step was to search databases for studies on Mobile learning and Medical Education research in SSA. Search terms such as “m-learning,” “m-health,” “e-health,” “mobile technologies,” “medical education,” “telemedicine,” “adoption,” “implementation,” “mobile learning,” and “Africa,” were explored in prominent databases such as Google Scholar, Science Direct, Scopus, IEEE, PubMed, Microsoft Academic, and Institutional database. Reference pages of retrieved articles were screened for relevant studies for the review materials. The obtained articles were then sorted based on inclusion, exclusion, and eligibility criteria, and set out for the review (see Table 1). While, Table 2 depicts the summary of the reviewed studies.
Table 1
Eligibility Criteria for the Systematic Review of Studies of M-Learning in Medical Education in SSA
| Inclusion criteria | Exclusion criteria |
|
|
|
|
|
|
|
|
|
|
Figure 1. PRISMA article selection flowchart.
Coding technique
Table 2
Summary of Reviewed Studies
| Author/ date | Paper title | Country | Research design & instrument | Sample & subjects | Statistical analysis adopted in the studies |
| Adebara et al. (2017) | Knowledge, Attitude and Willingness to Use mHealth Technology Among Doctors at a Semi-urban Tertiary Hospital in Nigeria | Nigeria | Quantitative. Questionnaire. | 220 medical doctors. | Descriptive and inferential statistics (Chi-square). |
| Anokwa (2010) | Delivering Better HIV Care in Sub-Saharan Africa Using Phone-Based Clinical Summaries and Reminders | Sub-Saharan Africa (SSA; Kenya). | Design of software framework that delivers summaries and reminders to HIV patients. | 4,500 patients. | Thematic narrative analysis. |
| Aryee (2014) | The Role of Mobile Phones in Health Education for Rural Communities in Ghana: An Exploratory Study in Digital Technologies | Ghana | Mixed Method (Questionnaire and interviews). | 92 health workers. | Descriptive statistics. |
| Barteit et al. (2015) | Self-Directed E-Learning at a Tertiary Hospital in Malawi -A Qualitative Evaluation & Lessons Learnt | Malawi | Qualitative study, using face-to-face interviews, guided group discussions, and observations. | 14 medical doctors, interns, and clinical officers. | Narrative analysis. |
| Bediang et al. (2013) | Computer Literacy and E-learning Perception in Cameroon: The Case of Yaounde Faculty of Medicine and Biomedical Sciences | Cameroon | Quantitative. Questionaire. | 307 students, residents, and lecturers. | Descriptive statistics and chi-square. |
| Biruk, Yilma, Andualem, & Tilahun (2014) | Health Professionals Readiness to Implement an Electronic Medical Record System at Three Hospitals in Ethiopia: A Cross-Sectional Study | Ethiopia | Quantitative Cross-sectional design. Questionnaire. | 606 medical health professionals. | Descriptive statistics, bivariate, and multivariate logistic regression. |
| Chang et al. (2012a) | Smartphone-Based Mobile Learning With Physician Trainees in Botswana | Botswana | Quasi-experimental design. | Trainee physicians (sample not specified) | Descriptive statistics. |
| Chang et al. (2012b) | Use of Mobile Learning by Resident Physicians in Botswana | Botswana | Quantitative. questionnaire. | Seven resident physicians | Descriptive statistics, and narrative analysis. |
| Feldacker et al. (2017) | Continuing Professional Development for Medical, Nursing, and Midwifery. Cadres in Malawi, Tanzania and South Africa: A Qualitative Evaluation | SSA (Malawi, Tanzania, and South Africa) | Mixed method (focus group discussion [FGD], key informant interview, and questionnaire). | 89 healthcare workers. | Descriptive statistics. |
| Gupta, Marsden, Oluka, Sharma, & Lucas (2017) | Lessons Learned from Implementing E-Learning for the Education of Health Professionals in Resource-Constrained Countries | Uganda | Qualitative, using a case study approach (key informant interviews). | Three universities in Uganda. | Thematic narrative analysis. |
| Ibrahim et al. (2014) | Use of Smartphones Among Medical Students in the Clinical Years at a Medical School in Sub-Sahara Africa: A Pilot Study | Nigeria | Quantitative cross-sectional study. Questionnaire. | 123 medical students. | Descriptive statistics. |
| Lazarus, et al. (2017) | Tablet Technology in Medical Education in South Africa: A Mixed Methods Study | South Africa | Mixed method/ questionaire, (open and closed-ended). | 178 medical students. | Descriptive statistics and thematic analysis. for the open-ended questionnaire. |
| Masika et al. (2015) | Use of Mobile Learning Technology Among Final Year Medical Students in Kenya | Kenya | Cross-sectional descriptive study. | 292 medical, nursing, pharmacy, and dental students. | Chi-square and t-test for bivariate analysis (regression). |
| Obi et al. (2018) | E-Learning Readiness From Perspectives of Medical Students: A Survey in Nigeria | Nigeria | Quantitative cross-sectional survey. Questionnaire. | 284 medical students. | Descriptive statistics, analysis of variance (ANOVA), correlation, and multiple regression. |
| Olajubu, Odukoya, & Akinboro, (2014) | LWAs Computational Platform for E-Consultation Using Mobile Devices: Cases From Developing Nations | Nigeria | Experimental study, the design, development, and testing of a light weight agent (lwa) in mobile devices used for medical e-consultation in vulnerable areas of SSA. | Sample and subjects not specified. | Descriptive narrative. |
| Pimmer et al. (2014) | Informal Mobile Learning in Nurse Education and Practice in Remote Areas: A Case Study From Rural South Africa | South Africa | Qualitative study (interview and content analysis). | 16 nurses, facilitators, and clinical managers. | Qualitative content analysis. |
| Urassa et al. (2018) | Addressing Knowledge Gaps among Nurses in Health Care in Tanzania: Use of Mlearning Platforms in Tanzania | Tanzania | Mixed method, questionnaire, and interview | 428 active and dormant mobile-device users among nurses, and nursing officers. | Descriptive statistics. |
| Witt et al. (2016) | The Role of Tablets in Accessing Information Throughout Undergraduate Medical Education in Botswana | Botswana | Mixed method. | 82 undergraduate medical students. | Descriptive statistics. |
*Note. Refer to the reference list for the full details of the publications in the table.
Table 3 presents the results on the geographical spread of articles on m-learning in medical education in Sub-Saharan Africa:
Table 3
Spread of Articles on M-Learning, M-Health, and Telemedicine in Medical Education in SSA
| Country | Subregion | No. of studies | % | No. of studies by subregion | % |
| Cameroon | Central Africa | 01 | 5.6 | 01 | 5.6 |
| Kenya | Eastern Africa | 02 | 11.1 | 04 | 22.2 |
| Tanzania | Eastern Africa | 01 | 5.6 | - | |
| Uganda | Eastern Africa | 01 | 5.6 | - | |
| Malawi | South-Eastern Africa | 01 | 5.6 | 01 | 5.6 |
| Botswana | Southern Africa | 03 | 16.6 | 05 | 27.8 |
| South Africa | Southern Africa | 02 | 11.1 | - | - |
| Sub-Saharan Africa | SSA | 02 | 11.1 | 02 | 11.1 |
| Ghana | Western Africa | 01 | 5.6 | 05 | 27.8% |
| Nigeria | Western Africa | 04 | 22.2 | - | |
| Total | 18 | 100% | 18 | 100% |
Table 3 shows that studies on m-learning spanned across nine countries with two studies that were on the state of m-learning in Sub-Saharan Africa in general, without country specification. Southern and western Africa had five studies, eastern Africa produced four, while central Africa and south-eastern Africa had a study each. Based on countries, Nigeria had four studies (22.2%) which were the highest number of studies followed by Botswana with three (16.6%). Kenya and South-Africa had two studies each, which is (11.1%). Tanzania, Uganda, Malawi, and Ghana had one study each (5.6%). The spread of the studies is in Figure 2.
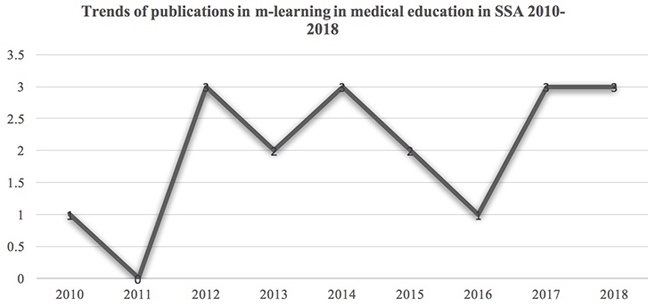
Figure 2. Trends of articles on m-learning in SSA 2010-2018.
The graphical details in Figure 2 show a relative consistency in the number of studies published on a yearly basis between 2010 and 2018. In 2011, there were no studies on m-learning in medical education, but the rest of the years had two studies, with a maximum of three studies recorded in 2018. In totality, this represents an average of one study per year for m-learning in medical education within the subregion.
Regarding research question three, the methodologies or approaches employed included; research design, data collection, subjects, sample size, and statistical tools used for the analysis.
The aspects of the methodology assessed were the research design and instruments adopted by the various studies, as presented in Table 4.
Table 4
Research Design and Instruments for the Reviews of M-Learning in Medical Education (ME) in SSA
| Design | No. of Studies | % | Instruments | ||
| Questionnaires | Interview | Both questionnaire & interview | |||
| Qualitative | 03 | 16.7% | 03(16.7%) | ||
| Quantitative | 07 | 38.8% | 07(38.8%) | ||
| Mixed Method | 05 | 27.8% | 05(27.7%) | ||
| Experimental (Feasibility/Pilot) | 03 | 16.7% | 03(16.7%) | ||
| Total | 18 | 100% | |||
Table 4 shows that a quantitative research design dominated most of the studies as seven (38.8%) out the total studies employed this research design, followed by the mixed method approach with five (27.8%), while qualitative and experimental design were the least used design. For data collection, the questionnaire was the most dominant instrument, used in seven studies representing 38.8%. A mixed method (i.e. survey and interview) was used in five studies (27.8%) while the least used research design was experimental (16.7%).
Subjects and Sample Size
The subjects selected for the studies and their corresponding sample sizes are featured in Table 5.
Table 5
Subjects and Sample Sizes
| Subjects format | No. of studies | % | Sample size | ||
| 100=Small | >150≤250=Medium | >250=Large | |||
| Medical doctors (instructors) | 02 | 11.1% | 01(5.55%) | - | 01(5.55%) |
| Trainee physicians, doctors (interns) students | 05 | 27.8% | 03(16.7%) | 01(5.56%) | 01(5.56%) |
| Both instructors (doctors) & medical students | 02 | 11.1% | 01(5.55) | - | 01(5.55%) |
| Doctors, health professionals including nurses (combined) | 06 | 33.3% | 03(16.65%) | -. | 03(16.65%) |
| Patients & institutions (experimental studies) | 03 | 16.6% | 02(11.1%) | - | 01(5.53%) |
| Total | 18 | 100% | 10 (55.5%) | 01(5.5%) | 07 (38.9%) |
Table 5 indicates that six studies (33.3%) used medical doctors, healthcare workers, and interns/ physician trainees as subjects of their studies, followed by five studies with trainee physicians and doctors only as their subjects. Two studies constituting 27.8%, used medical doctors only as their subjects (i.e. 11.1%), while another two studies used both instructors (doctors) and medical students (11.1%). Other studies that focused on medical institutions, in general, were experimental and based on pilot testing. This method constituted three studies (16.6%) of the total number of studies. With regards to sampling sizes, ten studies used small sample sizes (55.5%) while seven studies used large samples (38.9%), and only one study used medium size sample for their research. The results revealed that most of the studies used small sample sizes.
The quality and reliability of research findings lie with the analytical tools used for the analysis of the study. In that respect, this study sought to find out and aggregate the analytical tools used in the studies on m-learning in medical education in SSA as depicted in Table 6.
Table 6
Statistical Tools in the Research and Data Analysis
| Statistical tool | No. of studies | % |
| Thematic/ narrative | 05 | 27.7% |
| Descriptive | 08 | 44.4% |
| Correlation | 01 | 5.7% |
| Regression/Chi-square/GLMs/MANOVA | 04 | 22.2% |
| Structural equation modelling (SEM) | Nil | 00% |
| Total | 18 | 100% |
As shown in Table 6, eight studies (44.4%) used descriptive statistics, i.e. simple frequencies and percentages to analyse their data. Five studies used thematic and narrative analysis for their data analysis, especially for qualitative data. Four studies employed predictive and group difference analysis tools to analyse their data (22.2%). The least used statistical tool was a correlation which was featured in only one study (5.7%).
In response to research question four of this review, the study catalogued various factors reported across the reviewed studies as determinants or milestones of m-learning use or adoption. Results from the analysis produced ten elements and their frequencies of occurrence as represented in Figure 3.
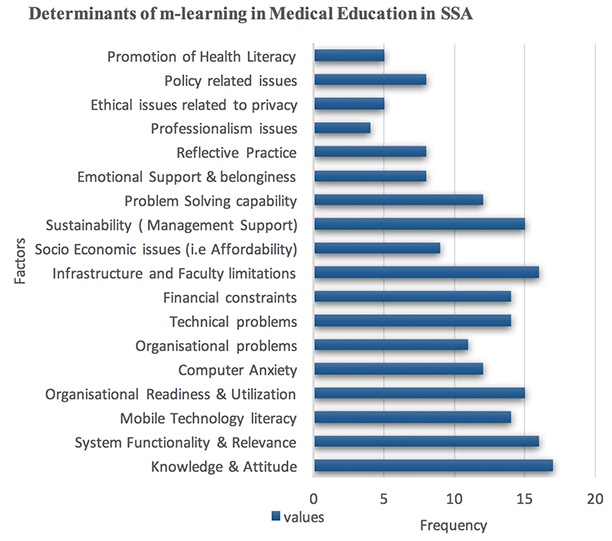
Figure 3. Determinants of m-learning in SSA.
Figure 3 represents the frequency of factors that determine the use and adoption of m-learning in Sub-Saharan Africa. Knowledge and attitude had the highest rate of occurrence of 17, followed by system functionality, relevance, and infrastructural and faculty limitations with 16. Organisational readiness and sustainability 15, mobile technology literacy, financial constraints, and technical problems had 14, while professionalism and ethical issues related to the use of m-learning had the least frequency of 4 and 5 respectively.
The outcome of problems in the reviewed studies is depicted in Figure 4.
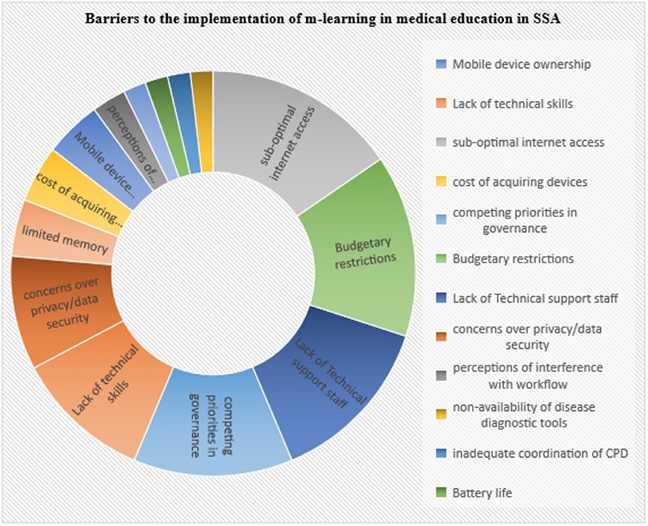
Figure 4. Sunburst chart of barriers to the implementation of m-learning in SSA.
Figure 4 highlights the challenges to effective implementation of m-learning in medical education in Sub-Saharan Africa. These challenges include: mobile device ownership; lack of technical skills; sub-optimal Internet access; cost of acquiring the devices; competing priorities in governance; budgetary restrictions; technical staff shortages; concerns over privacy; perception of interference with clinical workflow; absence of disease diagnostic tools; inadequate coordination of continuous professional development; battery life; small screen; and limited memory. Out of this broad range of challenges, 17 studies (94.4%) reported sub-optimal Internet access as a significant barrier, while 16 studies (88.9%) reported budgetary restrictions as a major hindrance to implementing m-learning in medical education in SSA. Fifteen studies (83%) said technical staff shortages was a barrier. Additionally, 14 (77.8%) reported competing priorities in governance as a determinant factor with 12 studies (66.7%) reporting a lack of technical skills. The least challenges in the reviewed studies include: battery life 2 (11.1%) and small screen 2 (11.1%).
The aggregate of the reviewed studies on m-learning in medical education in Sub-Saharan Africa indicated that western and southern Africa contributed more studies in m-learning in medical education. The outcome was because four studies were from Nigeria, and one was from Ghana, while Botswana and South Africa had three studies and two studies respectively. These subregions; southern and western Africa, are home to two of the most economically advanced countries in Africa as corroborated by Okai-Ugbaje, Ardzejewska, and Ahmed (2017) and Bervell and Umar (2017). The authors reported that world bank classification of countries in the region by income placed South Africa as an upper middle-income country while Ghana, Nigeria, Kenya, Tanzania, Uganda, and Botswana as lower-middle-income countries with potentials for further growth (Bervell & Umar, 2017). Since the significant determinants of effective implementation of technological innovation are infrastructure, financial constraints and competing priorities, possessing higher income means that the governments have committed enough resources in providing support for Information Technology and ICT resources in Higher Education. Consequently, this has resulted in more projects and research activities in e-learning and the integration of technologies in Higher Education, especially in medical education and practice.
Another reason for the seemingly encouraging interest in research on m-learning in medical education in Sub-Saharan Africa is the exponential rise in Internet penetration in the region (Anokwa, 2010). It is also instructive to note the relatively inexpensive features coupled with the affordances of mobile technologies also contributed to facilitating patient care and collaboration. Overall, the need to provide access to health services in remote and resource-constrained communities makes continuous research efforts in mobile technologies in medical education and practice defendable. Authors such as Chen et al. (2012), Feldacker et al. (2017), Pimmer et al. (2014), and Urassa et al. (2018), were all in agreement that m-learning programs have made significant impacts in places deployed. Furthermore, the World Health Organization (2011) reported that the quantum of mobile network penetration in SSA had surpassed infrastructure and Internet deployment. Nonetheless, higher income countries show more e-health activities than low-income countries. These advances may have culminated in the innovative application of mobile technologies to address health needs, thereby making the intersection of networked technology and health in developing countries become of utmost importance.
Instances of these remarkable innovative studies were in Ghana, where Aryee (2014) reported the practical use of mobile phones for inquiring about health concerns, practising teleconsultation, and for scrutinising counterfeit medications. The activity directly contributed to the successes recorded in the Mobile Doctors Network (MDnet) in 2009 (WHO, 2011). In a similar vein, Wasserman (2012) reported a significant increase in medical school enrolment in SSA which prompted the use of m-learning as a solution for providing easy access to learning materials and encouraging interaction amongst nurses in Tanzania. However, to have an effective continuous professional development program that will help in mitigating the impact of chronic diseases such as tuberculosis and HIV, there must be sustainable financial resources to provide the infrastructure that will lead to increased capacity and skills of the healthcare workers (Feldacker et al., 2017).
The results as presented in this study may be considered abysmal against the background that sub-Saharan Africa comprises of 48 countries out of which only nine states produced the number of reviewed articles (18). This supposedly indicates the low level of m-learning use in medical education in the subregion and holds promise for further research in that domain.
On models and designs adopted in research on m-learning, the review found out that there were no research models or conceptual models used in all the studies included in the report. Models are important because they provide powerful ways to address key information system research problems such as understanding information technology usage (Chin & Todd, 1995). Also, Borner (as cited in, Baltimore, Charo, & Kevles, 2016) asserts that models of technology and innovation help to inform policy decisions in education, health care, and other sectors which empower experts to make informed recommendations and predictions. Against this backdrop, model-based research will be constructive since m-learning is an attempt to improve the teaching and learning process in medical education, an approach that involves the use of mobile technologies for instructional, collaboration, and remote access to materials for just-in-time learning (Frehywot et al., 2013). However most of the studies in this review dwelled on practical solutions such as testing the effectiveness of smartphone (Android-based) applications with point-of-care programs for seeking medical information (Chang et al., 2012) and expert system developed to ease communication between doctors and health personnel across remote locations (Olajubu et al. 2014).
Regarding research design and instruments used in m-learning in medical education research in SSA, most of the reviewed studies applied the quantitative research design. Although the quantitative design is a standard measure and an excellent way of finalising results in the scientific field, its limitation is not accommodating findings that could augment the analysis Creswell (as cited in Bervell and Umar, 2017). However, a qualitative design was used in three of the studies, while a mixed method design was featured in five of the reviews. The authors are of the view that mixed method research approaches offer better ways to explain and understand the complexities of the organisational, social, and scientific phenomenon.
The study also revealed the use of all health personnel within the health care system as the most recurring subjects in the studies. This is understandably so as the interrelationship that exists between these actors in the implementation of any technology intervention in the health sector is critical to its success.
The dominant statistical tool adopted for data analysis in the studies on m-learning in medical education in SSA was descriptive statistics. The thematic narrative was the next most used statistical tool, and regression and Chi-square analysis appeared in only four studies. As outlined by Trochim (2006), descriptive statistics are used to describe the essential features of the data in a survey by porviding simple summaries about the sample and the measures. Using simple graphical analysis, they form the basis of virtually every quantitative analysis of data (Trochim, 2006). Perhaps, it is the most prevalent in health and medical research because it addresses visible and practical scientific evidence regarding what is or what the data shows or represents. However, relying only on descriptive statistics eliminates important relationships within mobile learning and even further makes it difficult in predicting the occurrence of other variable based on their predictors (Miles, Huberman, & Saldaña, 2014).
The significant determinants of m-learning in medical education implementation revealed were infrastructure and faculty limitations; competing priorities; budget constraints; system functionality and relevance; sustainability; socio-economic issues (affordability); promotion of health literacy; ethical issues related to privacy; emotional support and belongingness; knowledge and attitude; and mobile technology literacy and technical issues. Some of the studies reported on efforts to satisfy these factors or overcome the constraints. Gupta, Marsden, Oluka, Sharma, and Lucas (2017) suggested that to overcome issues of sub-optimal Internet connectivity (IT infrastructure) and network performance, intervention models like fair usage policy; network monitoring; effective enforcement of access regulations; and the use of user authentication systems should be adopted. For these interventions to succeed, there must be international solidarity and public/private partnerships to tackle the problems of shortage as recommended by Chenault (2011).
Recognising the critical role of evaluation on the success of policy implementation and change management across contexts, the WHO Global Observatory (2011) recommended continual evaluation of health systems, to come up with empirical evidence upon which policymakers, administrators and other stakeholders in SSA, can base their policy decisions. Investigating attitudes towards mobile technology in medical education, Adebara, Adebara, Olaide, Emmanuel, and Olanrewaju (2017), Ibrahim, Salisu, Popoola, and Ibrahim (2014), and Obi et al. (2018) reported participants demonstrated a positive attitude towards the of use mobile technology in medical education and practice. Conversely, this has a substantial effect on the acceptance of the technology and vice versa (Adebara et al., 2017; Ibrahim et al., 2014; Obi et al., 2018). However, the attitude of medical students and physicians or doctors is influenced by some specific factors such as; awareness, skills, training, and availability of the relevant infrastructure (Adebara et al., 2017; Ibrahim et al., 2014; Obi et al., 2018). With this, the success or otherwise of m-learning in medical education implementation in SSA depends on how to overcome the myriads of problems identified by the studies in the review.
Despite the challenges to the integration of mobile learning in health education in SSA, authors such as Pimmer et al. (2014) and Masita-Mwangi et al. (2012) identified the ways in which mobile learning contributes to health education such as; authentic problem solving; reflective practice; realisation of unpredictable teaching situations and lifelong learning. Mobile and smartphones support a broad range of educational practices in informal and clinical environments, especially for clinical examination and capturing of clinical events. Relating the outcome of their studies, Urassa et al. (2018) assert that mobile learning encourages more interaction in education and enhances self-directed learning. Adjorlolo and Ellingsen (2013) indicate that the use of mobile phones facilitates ICT support in patient care and collaborations that have their foundation on m-learning in health personnel training. This underscores the need for leadership across the Higher Education landscape, especially in medical education in sub-Saharan Africa, to do a comprehensive evaluation of the existing system. A thorough analysis of the research on ICT and technology-based solutions will inform decisions that will galvanise effort towards improved access and health care delivery at all levels (especially in resource-constrained communities). In furtherance of these objectives, Masika et al. (2015) recommends the public-private-partnership model, which considers the scarcity of resources in most SSA countries.
Based on the findings of the review the following recommendations are proposed:
This paper reviewed articles on mobile learning research trends and challenges to its implementation in medical education in SSA between 2010 to 2018. It identified the research designs, subjects, sample size, and instruments and statistical tools employed for the analysis in the studies. Additionally, the paper focused on the factors determining m-learning adoption and associated barriers to medical education in SSA. The study provided an overview of the state of the literature in that domain and sought to guide the direction of future studies, policy, and practice. Mtebe and Raphael (2018) opined that the proliferation of mobile phones in SSA and the emergence of fibre optical marine cable and adoption of various electronic learning systems would continue to increase, making the need for effective strategies to leverage these technologies very critical. However, we conclude this discussion anchoring on Traxler (2009)’s view on mobile learning: “mobile learning is uniquely suited to support context-specific and immediate learning, it is a major opportunity for distance learning since mobile technologies can situate learners and connect learners” (p.18). Mobile learning is indeed an opportunity for addressing the challenges of educational, social, political, and economic development of all resource constrained economies in general and of SSA in particular.
The authors acknowledge the contributions of all the authors of the literature used for the review. Authors are also grateful for the PhD sponsorship by Usmanu Danfodiyo University Sokoto and TETfund Nigeria for their support and encouragement.
Adebara, O., Adebara, I., Olaide, R., Emmanuel, G., & Olanrewaju, O. (2017). Knowledge, attitude, and willingness to use m-health technology among doctors at a semi-urban tertiary hospital in Nigeria. Journal of Advances in Medicine and Medical Research, 22(8), 1-10. Retrieved from http://www.journalrepository.org/media/journals/JAMMR_64/2017/Jul/Adebara2282017JAMMR33232.pdf
Adjorlolo, S., & Ellingsen, G. (2013). Readiness assessment for implementation of electronic patient record in Ghana: A case of University of Ghana hospital. Journal of Health Informatics in Developing Countries 7(2), 128-140. Retrieved from http://www.jhidc.org/index.php/jhidc/article/view/104
Africa-America Institute. (2015). AAI-SOE-report-2015-final. The State of Education in Africa Report 2015. Retrieved from http://www.aaionline.org/wp-content/uploads/2015/09/AAI-SOE-report-2015-final.pdf
Ally, M. (2009). Mobile learning is transforming the delivery of education and training. MIS Quarterly, 3(2), 137-152. doi: 10.1111/j.1467-8535.2007.00809.x
Anokwa, Y. (2010). Delivering better HIV care in sub-Saharan Africa using phone-based clinical summaries and reminders. America, 1-27. Retrieved from http://anokwa.com/publications/2010_UW_Generals_Paper.pdf
Aryee., K. L. (2014). The role of mobile phones in health education for rural communities in Ghana: An exploratory study in digital technologies. Retrieved from https://ir.lib.uwo.ca/etd/2030/
Baltimore, D., Charo, R. A., & Kevles, D. J. (2016). Summit on human gene editing. National Academies of Sciences, 61-69. Retrieved from https://www.nbp.pl/badania/seminaria/25x2016_2.pdf
Barteit, S., Hoepffner, P., Huwendiek, S., Karamagi, A., Munthali, C., Theurer, A., & Neuhann, F. (2015). Self-directed e-learning at a tertiary hospital in Malawi–A qualitative Evaluation and Lessons learnt. GMS Zeitschrift für medizinische Ausbildung [GMS journal for medical education], 32(1). doi: 10.3205/zma000949
Bediang, G., Stoll, B., Geissbuhler, A., Klohn, A. M., Stuckelberger, A., Nko’o, S., & Chastonay, P. (2013). Computer literacy and E-learning perception in Cameroon: the case of Yaounde Faculty of Medicine and Biomedical Sciences. BMC Medical Education, 13(1), 57. doi: 10.1186/1472-6920-13-57
Bervell, B., & Umar, I. N. (2017). A decade of LMS acceptance and adoption research in sub-Sahara African Higher Education: A systematic review of models, methodologies, milestones, and main challenges. Eurasia Journal of Mathematics, Science and Technology Education, 13(11), 7269-7286. doi: 10.12973/ejmste/79444
Biruk, S., Yilma, T., Andualem, M., & Tilahun, B. (2014). Health professionals’ readiness to implement electronic medical record system at three hospitals in Ethiopia: A cross sectional study. BMC medical informatics and decision making, 14(1), 115. doi: 10.1186/s12911-014-0115-5
Chang, A. Y., Littman-Quinn, R., Ketshogileng, D., Chandra, A., Rijken, T., Ghose, S. ... Kovarik, C. L. (2012a). Smartphone-based mobile learning with physician trainees in Botswana. International Journal of Mobile and Blended Learning, 4(2),1-14. doi: 10.4018/jmbl.2012040101
Chang, A. Y., Ghose, S., Littman-Quinn, R., Anolik, R. B., Kyer, A., Mazhani, L. ... & Kovarik, C. L. (2012b). Use of mobile learning by resident physicians in Botswana. Telemedicine and e-Health, 18 (1), 11-13. doi: 10.1089/tmj.2011.0050
Chen, C., Buch, E., Wassermann, T., Frehywot, S., Mullan, F., Omaswa, F., ... Olapade-Olaopa, E. O. (2012). A survey of sub-Saharan African medical schools. Human Resources for Health, 10(1), 4. doi: 10.1186/1478-4491-10-4
Chenault, J. (2011). Investigating and improving medical education and library resources at the Tamale teaching hospital in Northern Ghana : A case report. Kentucky Libraries, 76(2), 16-24. Retrieved from https://ir.library.louisville.edu/faculty/11
Chin, W. W., & Todd, P. A. (1995). On the use, usefulness, and ease of use of structural equation modelling in MIS research: A note of caution. MIS Quarterly, 19(2), 237-246. doi: 10.2307/249690
Creswell, J. W. (2013). Research design: Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, California, US: Sage Publications.
Feldacker, C., Pintye, J., Jacob, S., Chung, M. H., Middleton, L., Iliffe, J., & Kim, H. N. (2017). Continuing professional development for medical, nursing, and midwifery cadres in Malawi, Tanzania, and South Africa: A qualitative evaluation. PLoS ONE, 12(10), 1-16. doi: 10.1371/journal.pone.0186074
Frehywot, S., Vovides, Y., Talib, Z., Mikhail, N., Ross, H., Wohltjen, H., ... Scott, J. (2013). E-learning in medical education in resource-constrained low- and middle-income countries. Human Resources for Health, 11(1), 1. doi: 10.1186/1478-4491-11-4
Gupta, M., Marsden, S., Oluka, T., Sharma, R., & Lucas, H. (2017). Lessons learned from implementing E-learning for the education of health professionals in resource-constrained countries. Electronic Journal of E-Learning, 15(2), 144-155. Retrieved from http://www.ejel.org/volume15/issue2
Ibrahim, N. A., Salisu, M., Popoola, A. A., & Ibrahim, T. I. (2014). Use of smartphones among medical students in the clinical years at a medical school in Sub-Sahara Africa: A pilot study. Journal of Mobile Technology in Medicine, 3(2), 28-34. doi: 10.7309/jmtm.3.2.5
International Telecommunications Union. (2016). ICT facts and figures 2016. Retrieved from http://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2016.pdf
Kaliisa, R., & Picard, M. (2017). A systematic review of mobile learning in Higher Education: The African perspective. The Turkish Online Journal of Educational Technology, 16(1), 1-18. doi: 10.1017/CBO9781107415324.004
Koole, M. L. (2009). A model for framing mobile learning. In M. Ally (Ed.), Mobile learning: Transforming the delivery of education and training. (1(2), pp. 25-47). Edmonton, Canada: Athabasca University Press. Retrieved from https://books.google.com.ng/books?id=Itp60WteuJsC
Krull, G. E., & Duart, J. D. (2017). Research trends in mobile learning in Higher Education: A systematic review of articles (2011-2015). The International Review of Research in Open and Distributed Learning, 18(7), 1-23. doi: 10.19173/irrodl.v18i7.2893
Lazarus, L., Sookrajh, R., & Satyapal, K. S. (2017a). Tablet technology in medical education in South Africa: A mixed methods study. BMJ Open, 7(7), 1-10. doi: 10.1136/bmjopen-2016-013871
Masika, M. M., Omondi, G. B., Natembeya, D. S., Mugane, E. M., Bosire, K. O., & Kibwage, I. O. (2015). Use of mobile learning technology among final year medical students in Kenya. Pan African Medical Journal, 21, 1-12. doi: 10.11604/pamj.2015.21.127.6185
Masita-Mwangi, M., Mwakaba, N., Ronoh-Boreh, F., & Impio, J. (2012). Building a case for m-learning in Africa. Proceedings of the 2012 ACM Annual Conference Extended Abstracts on Human Factors in Computing Systems Extended Abstracts - CHI EA '12, 521. doi: 10.1145/2212776.2212827
Miles, M. B., Huberman, M. A., & Saldaña, J. (2014). Qualitative data analysis. A methods sourcebook. Zeitschrift Für Personalforschung [Journal For Personal Research], 28(4), 485-487. doi: 10.1136/ebnurs.2011.100352
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Prisma Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6(7), e1000097. doi: 10.1371/journal.pmed.1000097
Mtebe, J. S., & Raphael, C. (2018). Key factors in learners’ satisfaction with the e-learning system at the University of Dar es Salaam, Tanzania. Australasian Journal of Educational Technology, 34(4), 107-122. doi: 10.14742/ajet.2993
Naismith, L., Lonsdale, P., Vavoula, G., & Sharples, M. (2004). Literature review in mobile technologies and learning. Educational Technology, 11, 1-25. doi: ISBN:0-9548594-1-3
Obi, I. E., Charles-Okoli, A. N., Agunwa, C. C., Omotowo, B. I., Ndu, A. C., & Agwu-Umahi, O. R. (2018). E-learning readiness from perspectives of medical students: A survey in Nigeria. Nigerian Journal of Clinical Practice, 21(3), 293-300. doi: 10.4103/njcp.njcp_108_17
Okai-Ugbaje, S., Ardzejewska, K., & Ahmed, I. (2017). A systematic review of mobile learning adoption in Higher Education: The African perspective. I-manager's Journal on Mobile Applications and Technologies, 4(2), 1. doi: 10.26634/jmt.4.2.13830
Olajubu, E. A., Odukoya, O. H., & Akinboro, S. A. (2014). LWAs computational platform for e-consultation using mobile devices: Cases from developing nations. Technology and Health Care, 22(4), 561-571. doi: 10.3233/THC-140828
Organisation for Economic Co-operation and Development (OECD) (2009). Teaching practices, teachers’ beliefs and attitudes: Creating effective teaching and learning environments: first results from TALIS. OECD. doi: 10.1787/9789264068780-6-en
Oyo, B., & Kalema, B. M. (2014). Massive open online courses for Africa by Africa. The International Review of Research in Open and Distributed Learning, 15(6), 1-13. doi: 10.19173/irrodl.v15i6.1889
Pimmer, C., Brysiewicz, P., Linxen, S., Walters, F., Chipps, J., & Gröhbiel, U. (2014). Informal mobile learning in nurse education and practice in a remote areas: A case study from rural South Africa. Nurse Education Today, 34(11), 1398-1404. doi: 10.1016/j.nedt.2014.03.013
Traxler, J. (2009). The current state of mobile learning. In M. Ally (Ed.), Mobile learning: Transforming the delivery of education and training (Vol. 1, pp. 9-24). Edmonton, AB: Athabasca University Press.
Trochim, W. M. K. (2006). The research methods knowledge base (2nd ed.). Cincinnati, OH: Atomic Dog Publishing. doi: 10.2471/BLT.05.029181
Tsinakos, A., & Ally, M. (2013). Global mobile learning implementations and trends. Academia.Edu. Retrieved from http://www.academia.edu/download/36240447/global_Mobile_Learning.pdf#page=31%
Urassa, D., Chaya, P., & Pilot, J. (2018). Addressing knowledge gaps among nurses in healthcare in Tanzania: Use of m-learning platforms in Tanzania. Global Journal of Human Social Science 18(1), 54-61.
Witt, R. E., Kebaetse, M. B., Holmes, J. H., Ryan, L. Q., Ketshogileng, D., Antwi, C., ... Nkomazana, O. (2016a). The role of tablets in accessing information throughout undergraduate medical education in Botswana. International Journal of Medical Informatics. 88, 71-77. doi: 10.1016/j.ijmedinf.2016.01.006
World Health Organization. (2011). M-Health: New horizons for health through mobile technologies. Observatory, 3, 66-71. doi: 10.4258/hir.2012.18.3.231
Yunusa, A. A., & Dalhatu, I. I. (2014). Blended learning technique: Rethinking pedagogical approaches in sandwich / B.Ed art-time degree programmes in Nigerian universities. International Journal of Topical Issues in Education, Maiden Edition, 58-68. Retrieved from http://oer.udusok.edu.ng:8080/xmlui/handle/123456789/781

Octennial Review (2010-2018) of Literature on M-Learning for Promoting Distributed-Based Medical Education in Sub-Saharan Africa by Abdullahi Abubakar Yunusa, Irfan Naufal Umar, and Brandford Bervell is licensed under a Creative Commons Attribution 4.0 International License.